Kidney
Newsletter
Keeping you up to date with the latest exciting advances and discussions in nephrology
Clinical challenges in kidney disease management
The following irregularities contribute to the multifactorial nature of the pathophysiology of CKD-associated pruritus (CKD-aP):

Upregulated
inflammatory state1–6

Dysregulated endogenous
opioid system1–5

Peripheral
neuropathy1,3,5,7

Uremic
abnormalities1–5
by a chronic, systemic itch8,9
CKD-aP is common in patients on dialysis (up to 69%)10
37% experience moderate-to-severe pruritus10
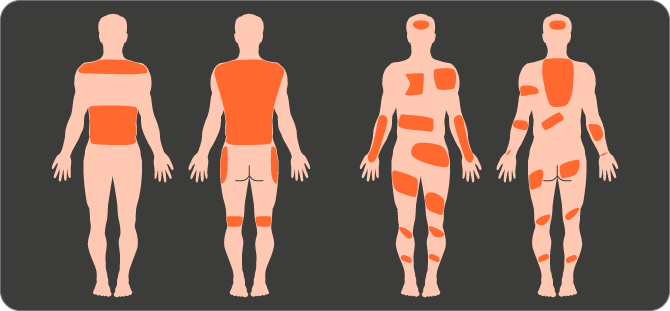
Pruritus distribution is highly variable from patient to patient11
Severe itching is typically bilateral, symmetrical, persistent and generalized11
Studies in dialysis patients have shown that CKD-aP:


likelihood of being diagnosed
with depression compared
with patients on hemodialysis
without CKD-aP11,12

work or maintain an
active social life10
Severe CKD-aP is also an independent predictor of mortality and hospitalization, related to an increased susceptibility to cardiovascular, infection and skin-related complications8,9,13
 Mortality
Mortality
 Hospitalization
Hospitalization
 Infection
Infection
What are the barriers to optimizing
clinical care across the ckd continuum?
Data suggest that CKD-aP is significantly under-recognized


by itchy skin” did not
report their symptoms
to an HCP10
Clinical management of CKD-aP is challenging as guidance is mostly restricted to broad dermatology guidelines and expert reviews14,15
- Antihistamines are the most commonly used systemic antipruritic drugs in dermatology, but are not recommended as a treatment option in CKD-aP due to a lack of proven efficacy15
- Off-label treatments have limited supporting evidence and adverse effects may limit their use in patients with CKD-aP16
FOOTNOTES
CKD-aP, chronic kidney disease-associated pruritus; HCP, healthcare professional.
REFERENCES
- Shirazian S, et al. Int J Nephrol Renovasc Dis 2017;10:11–6;
- Mettang T, Kremer A. Kidney Int 2015;87:685–91;
- Wang H, Yosipovitch G. Int J Dermatol 2010;49:1–11;
- Kuypers D. Nat Clin Pract Nephrol 2009;5:157–70;
- Patel T, et al. Am J Kidney Dis 2007;50:11–20;
- Kimmel M, et al. Nephrol Dial Transplant 2006;21:749–55;
- Zakrzewska-Pniewska B, et al. Neurophysiol Clin 2001;31:181–93;
- Narrita I, et al. Kidney Int 2006;69:1626–32;
- Ramakrishnan K, et al. Int J Nephrol Renovasc Dis 2014;7:1–12;
- Rayner H, et al. Clin J Am Soc Nephrol 2017;12:2000–17;
- Mathur V, et al. Clin J Am Soc Nephrol 2010;5:1410–9;
- Pisoni R, et al. Nephrol Dial Transplant 2006;21:3495–505;
- Sukul N, et al. Kidney Med 2020;3:42–53;
- Combs S, et al. Semin Nephrol 2015;35:383–91;
- Weisshaar E, et al. Acta Derm Venereol 2019;99:469–506;
- Verduzco H, Shirazian S. Kidney Int Rep 2020;5:1387–402.



 BACK TO OPTIONS
BACK TO OPTIONS